Summary / Abstract
The latest data of all-cause mortality by week does not show a winter-burden mortality that is statistically larger than for past winters. There was no plague. However, a sharp “COVID peak” is present in the data, for several jurisdictions in Europe and the USA. This all-cause-mortality “COVID peak” has unique characteristics:
- Its sharpness, with a full-width at half-maximum of only approximately 4 weeks;
- Its lateness in the infectious-season cycle, surging after week-11 of 2020, which is unprecedented for any large sharp-peak feature;
- The synchronicity of the onset of its surge, across continents, and immediately following the WHO declaration of the pandemic;
- and its USA state-to-state absence or presence for the same viral ecology on the same territory, being correlated with nursing home events and government actions rather than any known viral strain discernment.
These “COVID peak” characteristics, and a review of the epidemiological history, and of relevant knowledge about viral respiratory diseases, lead me to postulate that the “COVID peak” results from an accelerated mass homicide of immune-vulnerable individuals, and individuals made more immune-vulnerable, by government and institutional actions, rather than being an epidemiological signature of a novel virus, irrespective of the degree to which the virus is novel from the perspective of viral speciation.
The paper is organized into the following sections:
- Cause-of-death-attribution data is intrinsically unreliable
- Year-to-year winter-burden mortality in mid-latitude nations is robustly regular
- Why is the winter-burden pattern of mortality so regular and persistent?
- A simple model of viral respiratory disease de facto virulence
- All-cause mortality analysis of COVID-19
- Interpreting the all-cause mortality “COVID peak”
Cause-of-death-attribution data is intrinsically unreliable
Assignment of cause of death, with infectious diseases and comorbidity, is not only technically difficult (e.g., Simonsen et al., 1997; Marti-Soler et al., 2014) but also contaminated by physician-bias, politics and news media.
This has been known since modern epidemiology was first practiced. Here is Langmuir (1976) quoting the renowned pioneer William Farr, regarding the influenza epidemic of 1847:
Farr uses this epidemic to chide physicians mildly on their narrow views pointing out that sharp increases were observed not only in influenza itself but in bronchitis, pneumonia and asthma and many other non-respiratory causes, he states:
‘… there is a strong disposition among some English practitioners not only to localize disease but to see nothing but the local disease. Hence, although it is certain that the high mortality on record was the immediate result of the epidemic of influenza, the deaths referred to that cause are only 1,157.’
And, such bias is generally recognized by leading epidemiologists (Lui and Kendal, 1987):
… the decision to classify deaths into “pneumonia and influenza” is subjective and potentially inconsistent. On one hand, the effect of influenza or influenza-related pneumonia may be underestimated because underlying chronic diseases, particularly in the elderly, are usually noted as the cause of death on the death certificate. On the other hand, after influenza activity has been publicly reported there may be an increased tendency to classify deaths as due to “pneumonia and influenza,” thereby amplifying the rate of increase in P&I deaths or, when a decline in influenza activity is reported, a bias toward decreasing the classification of deaths related to “pneumonia and influenza” may result. Surveys to evaluate these possibilities have not been done.
One can reasonably expect that in the current world of social media, with a World-Health-Organization-declared (WHO-declared) “pandemic”, such bias will only be greater compared to its presence in past viral respiratory disease epidemics.
For example, it is difficult to interpret the synchronicity of the WHO declaration of COVID-19 as a pandemic and the onset of the observed surge in reported COVID-19 cases and deaths as being the product of either coincidence or extraordinary forecasting ability of the global health-monitoring system:
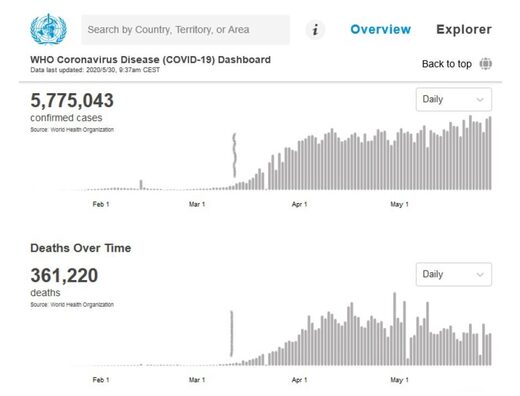
WHO data was accessed on 30 May 2020. The vertical lines in pencil indicate the date at which
the WHO declared the pandemic.
was accessed on 30 May 2020. The vertical line in pencil indicates the date at which the WHO
declared the pandemic.
Instead, in light of past epidemics, it is more likely that this remarkable synchronicity phenomenon arises from biased reporting, in the flexible context of using urgently manufactured laboratory tests that are not validated, clinical assessments of a generic array of symptoms, and tentative cause-of-death assignations of complex comorbidity circumstances.
That is why rigorous epidemiological studies rely instead on all-cause mortality data, which cannot be altered by observational or reporting bias (as discussed in Simonsen et al., 1997; and see Marti-Soler et al., 2014). A death is a death is a death.
Year-to-year winter-burden mortality in mid-latitude nations is robustly regular
Modern human mortality in mid-latitude temperate-climate regions is robustly seasonal. Graphs of number of all-cause deaths per unit of time (month, week, day), in given regions, have a yearly pattern, with a peak-to-trough amplitude of typically 10% to 30% of the trough-baseline value, largely irrespective of the specific pathogens that populate the specific seasons. High mortality occurs in winter, and is thus inverted in the Northern and Southern hemispheres (e.g., Marti-Soler et al., 2014).
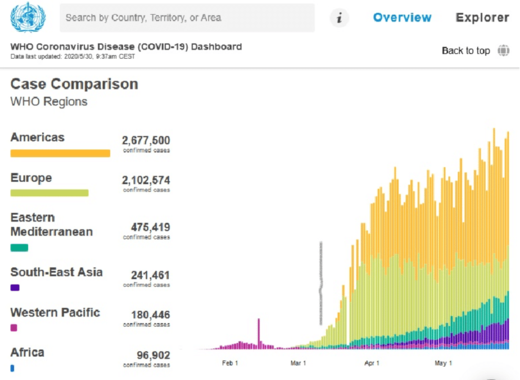
For the USA, the phenomenon is well illustrated in this figure from Simonsen et al. (1997):
their Fig. 1).
In such a graph, the area under a peak, to its trough-level baseline, is the total number of yearly winter-burden deaths above the trough baseline. The thus calculated yearly “excess” number of deaths, here (in the era 1972-1993), is always approximately 8% to 11% of the total yearly trough-baseline-level deaths, also approximately 8% to 11% of the yearly all-cause mortality.
This regular and seasonal “excess” mortality, or winter burden, has been an epidemiological challenge to understand, although, starting with Farr, many epidemiologists originally attributed it almost entirely to the seasonal influenza-like viral respiratory diseases.
Nonetheless, the agonizing difficulty of understanding the cause(s) of this remarkably regular and global (both hemispheres, but inverted) pattern persists, as illustrated by Marti-Soler et al. (2014) (references omitted):
Given that mortality from cancer showed virtually no seasonality pattern, the seasonality of overall mortality is driven mostly by seasonality of both CVD [cardiovascular diseases] and non-CVD/non-cancer mortality. For these conditions, and particularly for CVD, exposure to cold is a plausible explanation for the observed seasonality, given relationship of cold climate with latitude. Several longitudinal studies have demonstrated that a decrease in outdoor temperature was associated with a rise in all-cause mortality. However, other latitude-dependent factors, such as dietary habits, sun exposure (vitamin D levels) and human parasitic and infectious agents might also play a role.
The magnitude of the seasonal pattern for CVD mortality was higher than that for all-cause mortality. The seasonality of CVD mortality might be partly due to the joint seasonality of several known CVD risk factors, as described previously. Similarly, lifestyle factors such as diet and physical activity also tend to differ during summer and winter months. Moreover, exposure to cold increases energy expenditure, peripheral vasoconstriction and cardiac afterload, thus potentially triggering myocardial ischemia 6 and stroke. Finally, winter prone influenza infection might also be a trigger for CVD deaths by exacerbating CVD conditions or due to secondary complications. This is likely to be the case of concentration of air pollutants.
The seasonality of non-CVD/non-cancer mortality can relate to the facts that chronic obstructive pulmonary disease and pneumonia are frequent diseases in this category and that these disease are exacerbated by influenza, other influenza-like infections and concentrations of air pollutants, which are all more frequent in winter. A few other diseases in the non-CVD/non-cancer category also present a seasonal pattern, e.g. depression, suicide, and oesophageal variceal bleeding.
Why is the winter-burden pattern of mortality so regular and persistent?
Even the seasonality of the pneumonia and influenza (“P&I”) part alone (which is a large part of what Marti-Soler et al. quantify as “non-CVD/non-cancer mortality”) was not understood until a decade ago. Until recently, it was debated whether the P&I yearly pattern arose primarily because of seasonal change in virulence of the pathogens, or because of seasonal change in susceptibility of the host (such as from dry air causing tissue irritation, or diminished daylight causing vitamin deficiency or hormonal stress). For example, see Dowell (2001). In a sense, the answer is “neither”.
In a landmark study, Shaman et al. (2010) showed that the seasonal pattern of respiratory-disease (P&I) excess mortality can be explained quantitatively on the sole basis of absolute humidity, and its direct controlling impact on transmission of airborne pathogens.
Lowen et al. (2007) demonstrated the phenomenon of humidity-dependent airborne-virus contagiousness in actual disease transmission between guinea pigs, and discussed potential underlying mechanisms for the measured controlling effect of humidity.
The underlying mechanism is that the pathogen-laden aerosol particles or aerosol-size droplets are neutralized within a half-life that monotonically and significantly decreases with increasing ambient absolute humidity. This is based on the seminal work of Harper (1961). Harper experimentally showed that viral-pathogen-carrying droplets were inactivated within shorter and shorter times, as ambient absolute humidity was increased.
Harper argued that the viruses themselves were made inoperative by the humidity (“viable decay”), however he admitted that the effect could be from humidity-enhanced physical removal or gravitational sedimentation of the droplets (“physical loss”):
“Aerosol viabilities reported in this paper are based on the ratio of virus titre to radioactive count in suspension and cloud samples, and can be criticized on the ground that test and tracer materials were not physically identical.”
The latter (“physical loss”) seems more plausible to me, since absolute humidity would have a universal physical effect of causing particle/droplet growth-by-condensation and gravitational sedimentation (and, conversely, loss-by-evaporation and aerosolization), and all tested viral pathogens have essentially the same humidity-driven “decay”. Furthermore, it is difficult to understand how a virion (of any virus type) in a droplet would be molecularly or structurally attacked or damaged by an increase in ambient humidity. A “virion” is the complete, infective form of a virus outside a host cell, with a core of RNA or DNA and a capsid. No actual molecular or other mechanism of the humidity-driven intra-droplet “viable decay” of a virion postulated by Harper (1961) has, to date, been explained or studied, whereas gravitational sedimentation (“physical loss”) is well understood.
In any case, the explanation and model of Shaman et al. (2010) is not dependent on the particular mechanism of the absolute-humidity-driven decay of virions in aerosol/droplets. Shaman’s quantitatively demonstrated model of seasonal regional viral epidemiology is valid for either mechanism (or combination of mechanisms), whether “viable decay” or “physical loss”.
The breakthrough achieved by Shaman et al. is not merely some academic point. Rather, it has profound health-policy implications, which have been entirely ignored or overlooked in the current coronavirus pandemic:
- It means that the seasonality of P&I mortality is directly driven by absolute-humidity-controlled contagiousness of the viral respiratory diseases.
If my view of the mechanism is correct (i.e., “physical loss” rather than “viable decay”), then:
- It additionally implies that the transmission vector must be small aerosol particles in fluid suspension in air, breathed deeply into the lungs, indoors; not hypothesized routes such as actual fluid or fomite contact, and not large droplets and spit (that are quickly gravitationally removed from the air, or captured in the mouth and digestive system).
- And it means that social distancing, masks, and handwashing can have little effect in the actual epidemic spread during the winter season (see: Rancourt, 2020).
On the epidemiology modelling side, Shaman’s work implies that, rather than being a fixed number (dependent solely on the spatial-temporal structure of social interactions in a completely and variably susceptible population, and on the viral strain), the epidemic’s basic reproduction number (R0) is predominantly dependent on ambient absolute humidity. For a definition of R0, see HealthKnowlege-UK (2020): R0 is “the average number of secondary infections produced by a typical case of an infection in a population where everyone is susceptible.”
Shaman et al. showed that R0 must be understood to vary seasonally between humid-summer values of just larger than “1” and dry-winter values typically as large as “4” (for example, see their Table 2). In other words, the seasonal infectious viral respiratory diseases that plague temperate-climate regions every year go from being intrinsically mildly contagious to virulently contagious, due simply to the bio-physical mode of transmission controlled by atmospheric absolute humidity, largely irrespective of any other consideration.
Furthermore, indoor airborne virus concentrations have been shown to exist (in day-care facilities, health centres, and onboard airplanes) primarily as aerosol particles of diameters smaller than 2.5 μm, such as in the work of Yang et al. (2011):
“Half of the 16 samples were positive, and their total virus concentrations ranged from 5,800 to 37,000 genome copies m−3. On average, 64 percent of the viral genome copies were associated with fine particles smaller than 2.5 µm, which can remain suspended for hours. Modelling of virus concentrations indoors suggested a source strength of 1.6 ± 1.2 × 105 genome copies m−3 air h−1 and a deposition flux onto surfaces of 13 ± 7 genome copies m−2 h−1 by Brownian motion. Over 1 hour, the inhalation dose was estimated to be 30 ± 18 median tissue culture infectious dose (TCID50), adequate to induce infection. These results provide quantitative support for the idea that the aerosol route could be an important mode of influenza transmission.”
Such small particles (smaller than 2.5 μm) are part of air fluidity, are not subject to gravitational sedimentation, and can therefore be breathed deeply into the lungs.
The next question is: How many such pathogen-laden particles are needed to cause infection in a person of average immune-response capacity?
Yezli and Otter (2011), in their review of the minimal infective dose (MID), point out relevant features:
- most respiratory viruses are as infective in humans as in tissue culture having optimal laboratory susceptibility
- the 50%-probability MID (“TCID50”) has variably been found to be in the range 100−1000 virions
- there are typically 103−107 virions per aerolized influenza droplet with diameter 1 μm − 10 μm
- the 50%-probability MID easily fits into a single (one) aerolized droplet
For further background:
- A classic description of dose-response assessment is provided by Haas (1993).
- Zwart et al. (2009) provided the first laboratory proof, in a virus-insect system, that the action of a single virion can be sufficient to cause disease.
- Baccam et al. (2006) calculated from empirical data that, with influenza A in humans, “we estimate that after a delay of ~6 h, infected cells begin producing influenza virus 9 and continue to do so for ~5 h. The average lifetime of infected cells is ~11 h, and the half-life of free infectious virus is ~3 h. We calculated the [in-body] basic reproductive number, R0, which indicated that a single infected cell could produce ~22 new productive infections.”
- Brooke et al. (2013) showed that, contrary to prior modeling assumptions, although not all influenza-A-infected cells in the human body produce infectious progeny (virions), nonetheless, 90% of infected cell are significantly impacted, rather than simply surviving unharmed.
The above review means that all the viral respiratory diseases that seasonally plague temporal-climate populations every year are extremely contagious for two reasons: (1) they are transmitted by small aerosol particles that are part of the fluid air and fill virtually all enclosed air spaces occupied by humans, and (2) a single such aerosol particle carries the minimal infective dose (MID) sufficient to cause infection in a person, if breathed into the lungs, where the infection is initiated.
This is why the pattern of all-cause mortality is so robustly stable and distributed globally, if we admit that the majority of the burden is induced by viral respiratory diseases, while being relatively insensitive to the particular seasonal viral ecology for this operational class of viruses. This also explains why the pattern is inverted between the Northern and Southern hemispheres, irrespective of tourist and business air travel and so one.
Virologists and geneticists see viral strains, mutations, and species (Alimpiev, 2019) like a man with a hammer sees nails. Likewise, there are professional rewards for identifying new viral pathogens and describing new diseases. For these reasons, scientists have not seen the forest for the trees.
But the data shows that there is a persistent and regular pattern of winter-burden mortality that is independent of the details, and that has a well-constrained distribution of year to year number of excess deaths (approximately 8% to 11% of the total yearly mortality, in the USA, 1972 through 1993). Despite all the talk of epidemics and pandemics and novel viruses, the pattern is robustly constant.
An anomaly worthy of panic, and of harmful global socio-economic engineering, would need to consist of a naturally caused yearly winter-burden mortality that is statistically greater than the norm. That has not occurred since the unique flu pandemic of 1918 (Hsieh et al., 2006).
The three recent epidemics assigned as pandemics, the H2N2 pandemic of 1957, the H3N2 pandemic of 1968, and the H1N1 pandemic of 2009, were not more virulent (in terms of yearly winter-burden mortality) than the regular seasonal epidemics (Viboud et al., 2010; Viboud et al., 2006; Viboud et al., 2005). In fact, the epidemic of 1951 was concluded to be more deadly, on the basis of P&I data, in England, Wales and Canada, than the pandemics of 1957 and 1968 (Viboud et al., 2006).
A simple model of viral respiratory disease de facto virulence
In the face of the persistent and regular pattern of winter-burden mortality, one is tempted to propose that the specific (structural, molecular, and binding) properties of the particular respiratory disease viral pathogen are not as determinative of mortality as virologists suggest. Instead, it is possible that mortality, in a given population exposed to these highly contagious viral pathogens that invade the lungs, is predominantly controlled by the population’s distribution of immune-system capacity and preparedness.
A viral load enters the lungs. Once the viral antigen is recognized, an immune response is mounted.1 A dynamic “war” ensues between the virus reproducing and spreading by infecting cells on the lining of the lungs, and the immune system doing everything it can to identify, locate and destroy infected cells before the said infected cells successfully can be productive of the virus.
The immune response is extraordinarily demanding of the body’s metabolic energy resources (which is why you “feed a cold”, “rest”, and “stay warm”). The demand in metabolic energy is prioritized, and can compete with the demands of essential bodily functions and immune responses to other pathogens. This is why individuals with “aging” diseases and comorbidity conditions are particularly at risk: their rate of metabolic energy supply to the immune-system is limited by their co-conditions, and the demand is not met at a sufficiently high rate to win the “war”. See: Straub (2017); Bajgar et al. (2015).
In a simple view of the infection (which I propose for illustration), a given individual, having a given state of health, can only provide metabolic energy to the immune system up to some maximum rate of supply, during the crucial stage of the “war”. Call this “rate of energy supply for the immune response”: RS. RS is in units of energy per unit time, J/s, or calories per second. If RS is sufficient to “win the war”, and is sustained long enough, then the individual recovers from the infection, and the immune system stores a molecular memory of the viral antigen, which greatly reduces energy demand for future immune responses to attacks from the same or sufficiently similar virus. If RS is insufficient then the individual succumbs to the virus and dies.
Therefore, the seasonal virus can be characterized as having a virus-specific value of RS, RSv, which is the RS threshold for survival of the infected person. If RS > RSv, then the person recovers. If RS < RSv, then the person dies. The larger the RSv, the more virulent is the virus, and vice versa.
A given human population (national or regional) will have a given distribution of RS values associated with the individual members of the population.
Mathematically, this distribution can be represented as a probability density of RS values. A probability-density value has units of number of persons per unit interval of RS. The total area under the probability density curve is the population, of the nation or region.
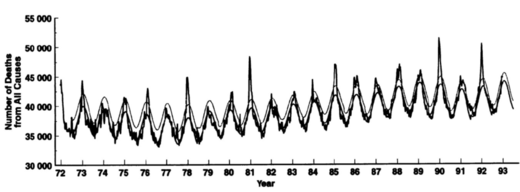
Figure 4 illustrates three hypothetical distributions of RS values, in three different populations of equal size. Here, “Germany” (solid-blue line) is for a current Western population, not having a particularly large elderly population; “Italy” (dashed-blue line) is for a current Western population having a large elderly population; and “Stressed” (solid-red line) is for a population of individuals subjected to high metabolic (or health) stress, such as might have been the case in 1918 England.
Such health stress can arise from nutritional deficiency, essential nutrient or vitamin efficiency, high levels of environmental stressor-agents, toxins, or pathogens, shelter deficiency (“fuel poverty”), oppressive working conditions, social-dominance oppression, substance abuse causing organ damage, and so on. There is a vast literature on these factors. As one anchor point, see: Sapolsky (2015); Sapolsky (2005).
Figure 4: Probability densities of RS values, for three populations of equal size but differing in health-stress levels and health vulnerabilities, as explained in the text. The three vertical lines, drawn in pencil and labelled “1”, “2” and “3”, show three different virus-specific values of RSv, as explained in the text. The hatched areas are the fractions (of total area) representing the mortality fractions for the less virulent virus having RSv value labelled “1”.
In this model, therefore, comparative mortality between populations, for a given viral pathogen, is determined by the different health states (distributions of RS values of the individuals) of the compared infected populations.
This is for the full cycle of infection and recovery. It says little about both the death rates on a daily basis and age distributions, which depend on the natural or forced spread of the infection, which in turn is not necessarily uniform in time and space but rather can target particular segments of the population, such as people confined in institutions.
Furthermore, the distribution of RS values for a given population can change significantly during the course of an epidemic, if vulnerable segments are subjected to additional health stressors, for example.
All-cause mortality analysis of COVID-19
In light of the above background and conceptual tools, we can now examine data for COVID-19, to date. For good reason (as per above), we ignore death-attributed data and model deconvolutions of P&I deaths versus other deaths deemed to be seasonal for reasons unrelated to the seasonal viral pathogens. We concentrate on all-cause mortality, by week.
All-cause mortality is not susceptible to bias, and is currently available for several jurisdictions. We use the raw data without any manipulation, and we do not modify the data to “correct” for changes in total population, or for changes in age structure of a population.
For the data, we rely on the CDC (USA), national institute data for England and Wales, and the graphical compilations of the EuroMOMO hub. We use only the latest weeks that are reported as complete (“>100%”, CDC) or reported to be of sufficient quality to publish. Unfortunately, some jurisdictions such as Canada can be characterized as slow and refractory to requests.
Figure 5 shows all-cause mortality by week for England and Wales, starting in 2010. The sudden single-week drops are book-keeping and death-certification-delay inconsistencies, which are counted in the following week(s). The red vertical line indicates the date at which the WHO declared the pandemic.
In declaring the pandemic, the WHO Director-General, Tedros Adhanom, put it this way, among other things:2
In the days and weeks ahead, we expect to see the number of cases, the number of deaths, and the number of affected countries climb even higher. […]
And we have called every day for countries to take urgent and aggressive action. We have rung the alarm bell loud and clear. […]
This is not just a public health crisis, it is a crisis that will touch every sector – so every sector and every individual must be involved in the fight.
I have said from the beginning that countries must take a whole-of-government, whole-of-society approach, built around a comprehensive strategy to prevent infections, save lives and minimize impact. […]
I remind all countries that we are calling on you to activate and scale up your emergency response mechanisms; Communicate with your people about the risks and how they can protect themselves – this is everybody’s business; Find, isolate, test and treat every case and trace every contact; Ready your hospitals; […] (my emphasis)
Adhanom’s words either were the most remarkable public health forecast ever made for England and Wales (and many jurisdictions in the world, see below), or something else might explain the sharp peak in all-cause mortality that immediately followed his declaration.
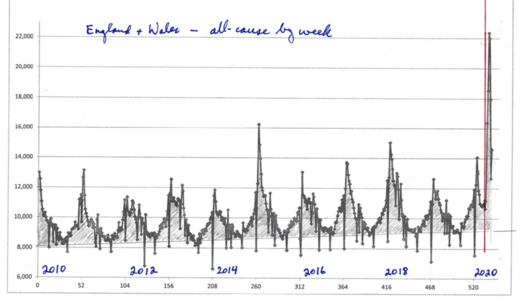
Figure 5: All-cause mortality by week for England and Wales, starting in 2010. The sudden single-week drops are book-keeping and death-certification-delay inconsistencies, which are counted in the following week(s). The red vertical line indicates the date at which the WHO declared the COVID-19 pandemic.
Importantly, the total number of winter-burden all-cause “excess” deaths for the season ending in 2020 (area above the summer baseline) is not statistically larger than for past years, and it remains to be seen how low the summer 2020 trough will be.
What can be called “the COVID peak” is a narrow feature (Figure 5). Relative to the summer baseline, the full-width at half-maximum of the peak is approximately 5 weeks. It has the distinction of being late in the infectious season, and of climbing far above the broader winter-burden hump.
This “COVID peak” is a unique event in the epidemiological history of England and Wales. Does this unique feature arise from an unusually novel viral pathogen, or does it arise from the unique, unprecedented and massive government response to the WHO declaration of a pandemic?
Note that such a “COVID peak” does not imply intrinsic virulence of the virus. It only means that the deaths of vulnerable persons, or persons made vulnerable, occurred in a short time span. For example, those who would have died in the next few or more weeks or months can have their deaths accelerated by human intervention, or those who are still recovering from a viral infection can be thrust into more precarious and stressful living conditions.
An analogous “COVID peak” occurred in the EuroMOMO hub data for Europe (Figure 6). Here again, the total number of winter-burden all-cause excess deaths for the season ending in 2020 (area above the summer baseline) is not statistically larger than for past years, and the date of declaration of the pandemic is shown by a vertical red line.
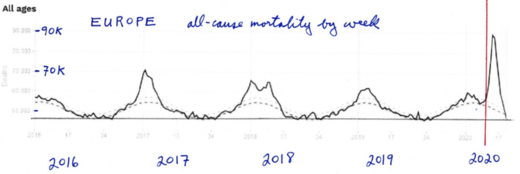
Figure 6: All-cause mortality by week EuroMOMO hub data for Europe, accessed on 1 June 2020. The date of declaration of the pandemic is shown by a vertical red line.
What looked like a concluding and “mild” 2020 season turned into a “COVID peak” immediately after the WHO declared the pandemic.
Let us next move to the USA, where both national and state-by-state current data is readily available, thanks to the CDC.
Figure 7 shows all-cause mortality by week for the USA, starting in 2014. Here the summer baseline is at approximately 46,000 to 52,000 deaths per week, increasing with the increase in total population. The red vertical line indicates the date at which the WHO declared the COVID-19 pandemic.
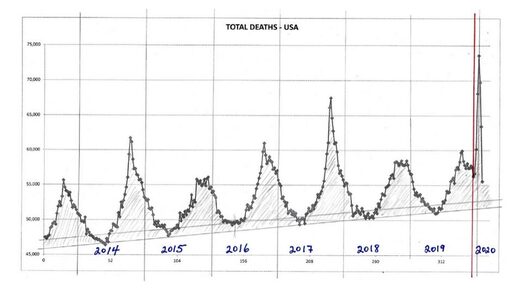
Figure 7: All-cause mortality by week for the USA, starting in 2014. The red vertical line
indicates the date at which the WHO declared the COVID-19 pandemic. The hatched or gray-fill areas represent the all-cause winter-burden deaths for each year.
Here, again, we see that the total number of winter-burden all-cause deaths for the season ending in 2020 (area above the summer baseline) is not statistically larger than for past recent years. There is no evidence, purely in terms of number of seasonal deaths, to suggest any catastrophic event or exceptionally virulent pathogen. There was no “plague”. The winter burden, in these years, is consistently in the range of approximately 6% to 9% of total yearly all-cause mortality, and the year to year variations are typical of historic variations.
On the other hand, there is again a “COVID peak”, which has the following unique features:
- It is remarkably sharp or narrow, having a full-width at half-maximum of the peak, relative to the summer baseline, of approximately only 4 weeks. By comparison, the sharp peaks in the infectious seasons ending in 2015 and 2018 have such full-widths of 14 and 9 weeks, respectively.
- It occurs later in the infectious season than any other large sharp peak ever seen for the USA, surging after week-11 of 2020.
- It surge occurs immediately after the WHO declared the pandemic, in perfect synchronicity, as seen in both Europe, and England and Wales, which are an ocean apart from the USA.
The “COVID peak” in the USA data arises from “hot spots”, such as New York City (NYC). Figure 8 shows the all-cause mortality by week for NYC, starting in 2013. The red vertical line indicates the date at which the WHO declared the COVID-19 pandemic.
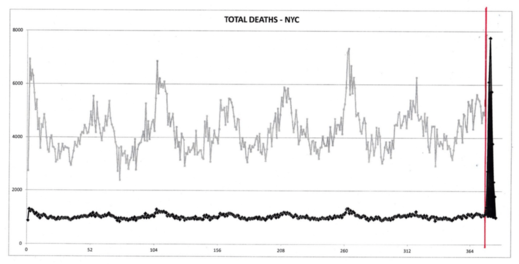
Figure 8: All-cause mortality by week for NYC, starting in 2013, in black. The red vertical line
indicates the date at which the WHO declared the COVID-19 pandemic. The grey line is simply
the same data on a vertically expanded and shifted scale, for visualization.
The NYC data makes no epidemiological sense whatsoever. The “COVID peak” here, on its face, cannot be interpreted as a normal viral respiratory disease process in a susceptible population. Local effects, such as importing patients from other jurisdictions or high densities of institutionalized or housed vulnerable people, must be in play, at least.
What is also striking is that some of the largest-population states in the USA, having large numbers of measured and reported cases, and large numbers of individuals with the antibodies, do not show a “COVID peak”. (Characteristic antibodies are produced and stored in the bodies of individuals who were infected and recovered following their immune responses. For example, see the antibody field study for California done by Bendavid et al., 2020).
This is shown for California in Figure 9, and for Texas in Figure 10.
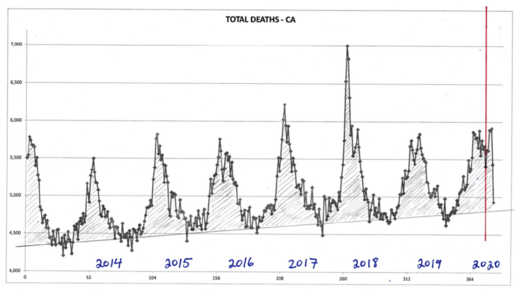
Figure 9: All-cause mortality by week for California, starting in 2013. The red vertical line
indicates the date at which the WHO declared the COVID-19 pandemic. The hatched or gray-fill areas represent the all-cause winter-burden deaths for each year.
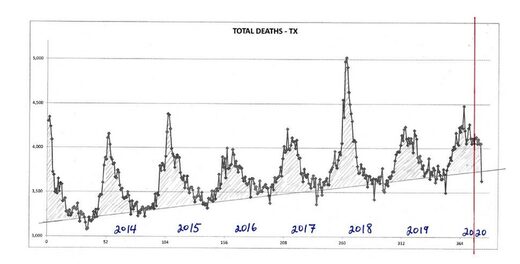
Figure 10: All-cause mortality by week for Texas, starting in 2013. The red vertical line indicates the date at which the WHO declared the COVID-19 pandemic. The hatched or gray-fill areas represent the all-cause winter-burden deaths for each year.
Also, none of the seven states that did not impose a lockdown (Iowa, Nebraska, North Dakota, South Dakota, Utah, Wyoming, and Arkansas) have a “COVID peak”.
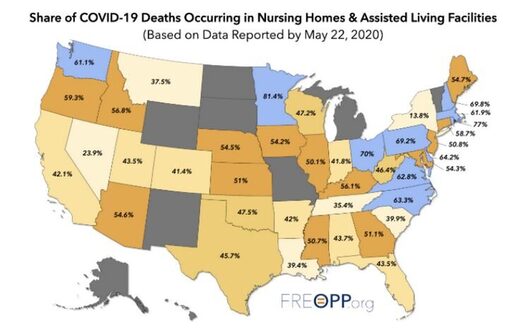
The presence of a “COVID peak” is positively correlated with the share of COVID-19-assigned deaths occurring in nursing homes and assisted living facilities, as per this map:
Interpreting the all-cause mortality “COVID peak”
Given the uniqueness of the all-cause mortality “COVID peak”:
- Its sharpness, with a full-width at half-maximum of only approximately 4 weeks;
- Its lateness in the infectious-season cycle, surging after week-11 of 2020, which is unprecedented for any large sharp-peak feature;
- The synchronicity of the onset of its surge, across continents, and immediately following the WHO declaration of the pandemic;
- and its USA state-to-state absence or presence for the same viral ecology on the same territory being correlated with nursing home events and government actions rather than any known viral strain discernment.
Given the above review of knowledge about seasonal viral respiratory diseases:
- The robustly persistent and regular winter-burden patterns of all-cause mortality, across the modern era of epidemiology, and across nations in two hemispheres;
- The newfound (2010) understanding that transmissivity is controlled by absolute humidity, and that the transmission vector is small aerosol particles taken deeply into the lungs;
- The increasing recognition of metabolic energy budgeting as the paradigm for understanding death from infectious diseases with comorbidity conditions, while recognizing that the immune system has hierarchical control over metabolic energy budgeting, second only to cognition of external imminent danger;
- and the increasing understanding of the dominant role of metabolic stress (including stress cognition, perceived stress) in depressing immune system response capacity.
I postulate that the “COVID peak” represents an accelerated mass homicide of immune-vulnerable individuals, and individuals made more immune-vulnerable, by government and institutional actions, rather than being an epidemiological signature of a novel virus, irrespective of the degree to which the virus is novel from the perspective of viral speciation.
Finally, my interpretation of the “COVID peak” as being a signature of mass homicide by government response is supported by several institutional documents, media reports, and scientific articles, such as the following examples. Two scientific articles are on-point:
- Hawryluck et al. (2004), on posttraumatic stress disorder (PTSD) arising from medical quarantine.
- Richardson et al. (2020), on statistical proof that mechanical ventilators killed critical COVID-19 patients.
*******
Media articles and institutional memos
“New study finds nearly all coronavirus patients put on ventilators died”, News Break | The Hill 04-23, 23 April 2020.
“New health care data suggests that almost half of all coronavirus patients placed on ventilators die, first reported by CNN. The data was gathered at Northwell Health, New York state’s largest hospital system. It revealed that about 20 percent of COVID-19 patients passed away, and 88 percent of those placed on ventilators died.”
“Daughter blames ‘chaos’ of COVID-19 pandemic for mother’s rapid decline”, by Arthur White-Crummey, Regina Leader-Post, 29 May 2020.
“Sue Nimegeers’s mother never had COVID-19, but she still counts her as a victim of the disease. “She never tested positive, but the chaos of the pandemic itself around us, we feel, took her from us just way too soon,” Nimegeers told the board of the Saskatchewan Health Authority (SHA) on Friday.”
“‘Deeply disturbing’ report into Ontario care homes released”, BBC, 27 May 2020.
“Mr Ford said a full investigation has been launched into the allegations, which included claims that facilities smelt of rotten food, infested with cockroaches and flies, and that elderly people were left for hours “crying for help with staff not responding”.”
“Nothing can justify this destruction of people’s lives”, Yoram Lass, former director of Israel’s Health Ministry, on the hysteria around Covid-19, sp!ked, 22 May 2020.
“Yoram Lass: It is the first epidemic in history which is accompanied by another epidemic – the virus of the social networks. These new media have brainwashed entire populations. What you get is fear and anxiety, and an inability to look at real data. And therefore you have all the ingredients for monstrous hysteria. It is what is known in science as positive feedback or a snowball effect. The government is afraid of its constituents. Therefore, it implements draconian measures. The constituents look at the draconian measures and become even more hysterical.”
“Cuomo downplays calls for federal probe into nursing home coronavirus deaths: ‘Ask President Trump’ “, by Andrew O’Reilly | Fox News, 20 May 2020.
“New York Gov. Andrew Cuomo on Wednesday brushed off calls for the Department of Justice to open an investigation into the massive number of deaths in the state’s nursing homes during the coronavirus pandemic – claiming he was only following guidelines from the Trump administration and Centers for Disease Control and Prevention. While no formal probe has been announced, the speculation comes amid scrutiny of his March 25 directive that required nursing homes to take on new patients infected with COVID-19.”
DATE: March 25, 2020
TO: Nursing Home Administrators, Directors of Nursing, and Hospital Discharge Planners
FROM: New York State Department of Health Advisory: Hospital Discharges and Admissions to Nursing Homes (Removed from: coronavirus.health.ny.gov)
“During this global health emergency, all NHs must comply with the expedited receipt of residents returning from hospitals to NHs. Residents are deemed appropriate for return to a NH upon a determination by the hospital physician or designee that the resident is medically stable for return. […] No resident shall be denied re-admission or admission to the NH solely based on a confmned or suspected diagnosis ofCOVID-19. NHs are prohibited from requiring a hospitalized resident who is determined medically stable to be tested for COVID-19 prior to admission or readmission.”
“Nursing Homes & Assisted Living Facilities Account for 42% of COVID-19 Deaths: A startling statistic has profound implications for the way we’ve managed the coronavirus pandemic”, by Gregg Girvan, FREOPP, 7 May 2020.
“Based on a new analysis of state-by-state COVID-19 fatality reports, it is clear that the most underappreciated aspect of the novel coronavirus pandemic is its effect on a specific population of Americans: those living in nursing homes and assisted living facilities.”
“Guilty – Of Breathing”, by Tony Heller, Tony Heller YouTube Channel, 24 May 2020.
“Lockdowns were sold months ago on the idea of ‘flattening the curve’. In most places there never was much of a curve to flatten, yet the lockdowns are still in place. Tens of millions are now having their lives destroyed – for the crime of breathing.”
“The ‘massacre’ of Italy’s elderly nursing home residents: Covid-19 patients in Italy’s virus epicentre of Lombardy were transferred to nursing homes by an official resolution with catastrophic consequences”, by Maria Tavernini and Alessandro Di Rienzo, TRT World, 20 April 2020.
“Hosting Covid-19 patients in nursing homes was like lighting a match in a haystack.”
“Coronavirus Update: How shoring up hospitals for COVID-19 contributed to Canada’s long-term care crisis”, by Jessie Willms and Hailey Montgomery, Globe & Mail, 20 May 2020.
“Most of the nursing- and retirement-home residents who have succumbed to COVID-19 in Canada died inside the virus-stricken, understaffed facilities as hospital beds sat empty.”
“There Is No Evidence Lockdowns Saved Lives. It Is Indisputable They Caused Great Harm”, by Briggs, wmbriggs.com, 14 May 2020.
“In the end, it does not come down to country- or even city-level statistics. It comes down to people. Each individual catches the bug or not, lives or dies. Not because of their country, but because of themselves, their health, their circumstances. Any given individual might have benefited from self-quarantine and loss of job. Just as any given individual might have come to a bad end from a lockdown.”
“Hospitals get paid more to list patients as COVID-19”, by Tom Kertscher, POLITIFACT, 21 April 2020.
“It’s standard for Medicare to pay a hospital roughly three times as much for a patient who goes on a ventilator, as for one who doesn’t. Medicare is paying a 20% add-on to its regular hospital payments for the treatment of COVID-19 victims. That’s a result of a federal stimulus law.”
“CDC: 80,000 people died of flu last winter in U.S., highest death toll in 40 years”, by Associated Press, STAT News, 26 September 2018.
“An estimated 80,000 Americans died of flu and its complications last winter — the disease’s highest death toll in at least four decades. The director of the Centers for Disease Control and Prevention, Dr. Robert Redfield, revealed the total in an interview Tuesday night with The Associated Press.”
Footnotes
- ‘The immune system: Cells, tissues, function, and disease’, medically reviewed by Daniel Murrell, MD on January 11, 2018 — Written by Tim Newman, at medicalnewstoday.com, accessed on 1 June, 2020.
- WHO Director-General’s opening remarks at the media briefing on COVID-19 – 11 March 2020
Scientific references
Alimpiev, Egor (2019) “Rethinking the Virus Species Concept”, dated 15 March 2019, posted to stanford.edu
Baccam, P. et al. (2006) “Kinetics of Influenza A Virus Infection in Humans”, Journal of Virology Jul 2006, 80 (15) 7590-7599; DOI: 10.1128/JVI.01623-05
Bajgar et al. (2015) “Extracellular Adenosine Mediates a Systemic Metabolic Switch during Immune Response”, PLoS Biol 13(4): e1002135.
Bendavid et al. (2020) “COVID-19 Antibody Seroprevalence in Santa Clara County, California”, medRxiv 2020.04.14.20062463
Brooke, C. B. et al. (2013) “Most Influenza A Virions Fail To Express at Least One Essential Viral Protein”, Journal of Virology Feb 2013, 87 (6) 3155-3162; DOI: 10.1128/JVI.02284-12
Dowell, S. F. (2001) “Seasonal variation in host susceptibility and cycles of certain infectious diseases”, Emerg Infect Dis. 2001;7(3):369-374. doi:10.3201/eid0703.010301
Haas, C.N. et al. (1993) “Risk Assessment of Virus in Drinking Water”, Risk Analysis, 13: 545-552. doi:10.1111/j.1539-6924.1993.tb00013.x
Harper, G J. (1961) “Airborne micro-organisms: survival tests with four viruses”, The Journal of Hygiene, vol. 59,4: 479-86. doi:10.1017/s0022172400039176
Hawryluck, L. et al. (2004) “SARS control and psychological effects of quarantine, Toronto, Canada”, Emerging Infect Dis., vol. 10,7: 1206-12. doi:10.3201/eid1007.030703
HealthKnowlege-UK (2020) “Charter 1a – Epidemiology: Epidemic theory (effective & basic reproduction numbers, epidemic thresholds) & techniques for analysis of infectious disease data (construction & use of epidemic curves, generation numbers, exceptional reporting & identification of significant clusters)”, HealthKnowledge.org.uk, accessed on 2020-04-10.
Hsieh, Y.C. et al. (2006) “Influenza pandemics: past, present and future”, J Formos Med Assoc. 105(1):1-6. doi:10.1016/S0929-6646(09)60102-9
Langmuir, A.D. (1976) “William Farr: Founder of Modern Concepts of Surveillance”, International Journal of Epidemiology, Volume 5, Issue 1, March 1976, Pages 13-18,
Locey and Lennon (2016) “Scaling laws predict global microbial diversity”, Proceedings of the National Academy of Sciences, May 2016, 113 (21) 5970-5975; DOI: 10.1073/pnas.1521291113
Lowen, A. C. et al. (2007) “Influenza Virus Transmission Is Dependent on Relative Humidity and Temperature”, PLoS Pathog 3(10): e151.
Lui, K.J., Kendal, A.P. (1987) “Impact of influenza epidemics on mortality in the United States from October 1972 to May 1985”, Am J Public Health, 77(6):712-716. doi:10.2105/ajph.77.6.712
Marti-Soler, H. et al. (2014) “Seasonal Variation of Overall and Cardiovascular Mortality: A Study in 19 Countries from Different Geographic Locations”, PLoS ONE, 9(11): e113500.
Rancourt, D.G. (2020), “Masks Don’t Work: A review of science relevant to COVID-19 social policy”, Technical Report, Research Gate, 10 April 2020, DOI: 10.13140/RG.2.2.14320.40967/1
Richardson, S. et al. (2020) “Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area”, JAMA. 323(20):2052-2059. doi:10.1001/jama.2020.6775
Sapolsky (2005) “The Influence of Social Hierarchy on Primate Health”, Science, 29 April 2005, vol. 308, pages 648-652. DOI: 10.1126/science.1106477
Sapolsky (2015), “Stress and the brain: individual variability and the inverted-U”, Nature Neuroscience, October 2015, vol. 18, no. 10, pages 1344-1346. doi: 10.1038/nn.4109.
Shaman, J. et al. (2010) “Absolute Humidity and the Seasonal Onset of Influenza in the Continental United States”, PLoS Biol 8(2): e1000316. https://doi.org/10.1371/journal.pbio.1000316
Simonsen, L. et al. (1997) “The impact of influenza epidemics on mortality: introducing a severity index”, Am J Public Health. 87(12):1944-1950. doi:10.2105/ajph.87.12.1944
Straub RH. (2017) “The brain and immune system prompt energy shortage in chronic inflammation and ageing”, Nat Rev Rheumatol. 13(12):743-751. doi:10.1038/nrrheum.2017.172
Viboud, C. et al. (2010) “Preliminary Estimates of Mortality and Years of Life Lost Associated with the 2009 A/H1N1 Pandemic in the US and Comparison with Past Influenza Seasons”, PLoS currents, vol. 2 RRN1153. 20 Mar. 2010, doi:10.1371/currents.rrn1153
Viboud C. et al. (2006) “Transmissibility and mortality impact of epidemic and pandemic influenza, with emphasis on the unusually deadly 1951 epidemic”, Vaccine. 24(44-46):6701-6707. doi:10.1016/j.vaccine.2006.05.067 handelgroup.publichealth.uga.edu
Viboud, C. et al. (2005) “Multinational Impact of the 1968 Hong Kong Influenza Pandemic: Evidence for a Smoldering Pandemic”, The Journal of Infectious Diseases, Volume 192, Issue 2, 15 July 2005, Pages 233-248,
Yang, W. et al. (2011) “Concentrations and size distributions of airborne influenza A viruses measured indoors at a health centre, a day-care centre and on aeroplanes”, Journal of the Royal Society, Interface. 2011 Aug;8(61):1176-1184. DOI: 10.1098/rsif.2010.0686.
Yezli, S., Otter, J.A. (2011) “Minimum Infective Dose of the Major Human Respiratory and Enteric Viruses Transmitted Through Food and the Environment”, Food Environ Virol 3, 1-30.
Zwart, M. P. et al. (2009) “An experimental test of the independent action hypothesis in virus-insect pathosystems”, Proc. R. Soc. B. 2762233-2242



His analysis of this past winter’s all-cause mortality rates, and his conclusion, is in line with ours:
And so, to summarize the ‘Covid-19 pandemic’ once more…
For two/three months the WHO, the media, and whichever ‘secret cabal’ controls both, shoved in everyone’s faces the fact that old people die when they reach the end of their lives. In the process of ‘making everyone realize the horror’ of this fact, irresponsible (and frankly pathological) elites willfully enjoined the general population to accelerate the deaths of tens of thousands of elderly and immune-compromised people, who died alone when separated from loved ones and abandoned by their regular healthcare practitioners.
Govt policy decisions – specifically, ONE ‘central’ govt policy decision, one followed by most Western govts, along with a few others – generated a ‘bottleneck of deaths’ by temporarily lifting the normal healthcare options available to society’s most vulnerable. These vulnerable people then died in droves, earlier than they would otherwise have done, and their deaths provided the media with images of ‘overflowing morgues’, crematoria, etc. from around the world.
Ironically then, the declared purpose of the lockdown – to ‘save the elderly’ by ‘flattening the curve’ – produced precisely the opposite outcome: the elderly were killed off, thereby artificially and precipitately spiking the otherwise flatter regular winter season curve.